Transcranial Magnetic Stimulation (TMS) offers a modern, non-invasive approach to treating certain mental health conditions by utilizing electromagnetic technology. TMS is approved by the FDA to treat major depressive disorder and obsessive-compulsive disorder, especially for patients who find little success with traditional treatments.
Across the nation and in specialized regional clinics—like those offering TMS in Nevada—this therapy has gained traction as a promising option for those seeking relief from persistent mental health symptoms.
As research and clinical applications advance, TMS becomes increasingly accessible to more people seeking alternative approaches to mental health care. In clinical settings, it is prized for its non-invasive nature and minimal side effects, setting it apart from many pharmaceutical interventions and more invasive therapies.
The Physics Behind TMS
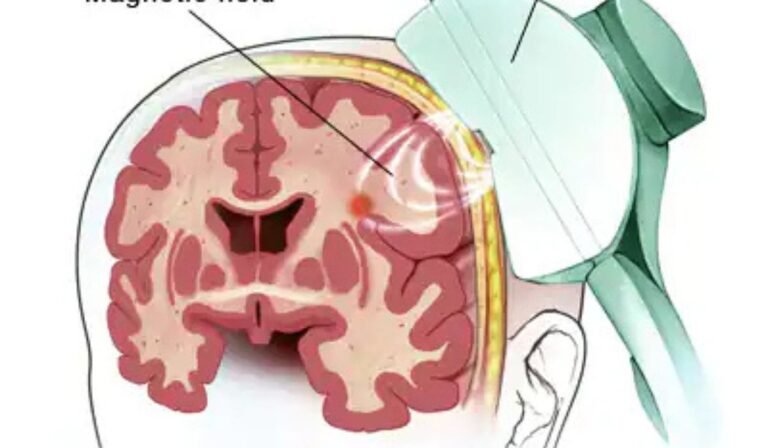
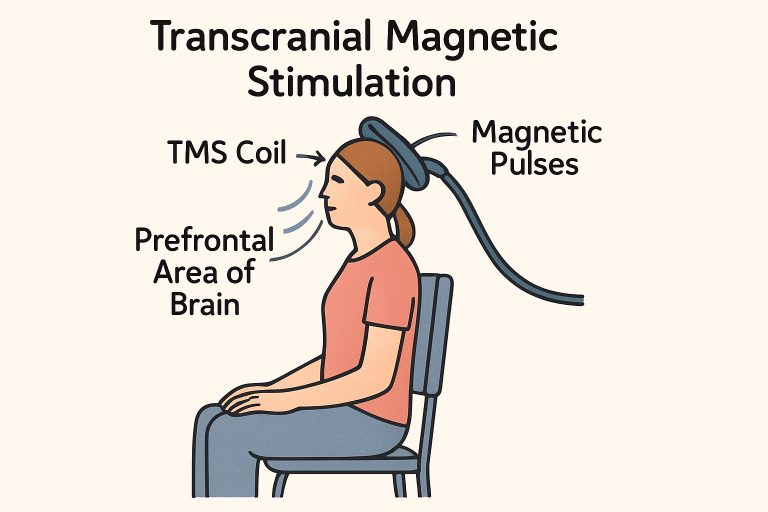
TMS operates through the principle of electromagnetic induction. During a session, a specially designed coil is placed gently against the patient’s scalp. This coil emits brief magnetic pulses, similar in power to those in MRI machines, which penetrate the scalp and skull, inducing a small electric current in the underlying brain tissue.
The precise control of these pulses allows clinicians to stimulate specific parts of the brain associated with mood and behavior. As shown in scientific literature, this localized stimulation can depolarize neurons or modulate existing neuronal circuits, offering the potential to alter dysfunctional brain activity linked to depression and other disorders.
According to Harvard Health, TMS has been increasingly recognized as an effective option for patients whose depression does not respond to medication, highlighting both its efficacy and non-invasive nature.
The safety profile of TMS is largely attributed to the nature of these magnetic fields, which do not cause lasting changes to non-targeted tissues and do not require anesthesia or sedation. By using focused coils and refined protocols, clinicians can repeatedly target relevant brain regions with high precision.
Targeting the Prefrontal Cortex
The dorsolateral prefrontal cortex (DLPFC) is the main target in TMS therapy for depression. This region is involved in regulating mood, decision-making, and executive function. Research indicates that people experiencing depression often show decreased activity in the DLPFC, which might contribute to persistent negative mood and cognitive symptoms.
By stimulating this area, TMS is designed to normalize brain activity, thereby helping to restore balance in the networks that control mood and thought patterns.
Beyond depression, TMS is now being investigated for its potential to address other neuropsychiatric and neurological conditions by targeting different brain regions and tailoring stimulation parameters accordingly. Clinical protocols are highly customizable, enhancing the potential effectiveness for individuals with different symptoms and diagnoses.
Neuroplasticity and TMS
An important mechanism underlying the benefits of TMS is neuroplasticity—the brain’s ability to reorganize itself by forming new neural connections. Repeated TMS sessions encourage the brain to modify neural pathways, supporting healthier patterns of brain activity over time. Research shows that this process may strengthen synaptic connections and facilitate recovery from depression by promoting more adaptive neural communication.
Both clinical and laboratory studies find that, with an adequate number of sessions, TMS may produce long-term improvements rather than just transient symptom relief. This adaptability is critical in conditions like depression, where disrupted neural networks contribute to persistent symptoms.
Clinical Evidence Supporting TMS
Large-scale clinical trials and meta-analyses have demonstrated the efficacy of TMS for people with treatment-resistant depression. The American Psychiatric Association endorses TMS as an option for patients who have not responded to standard therapies.
Some studies indicate response rates of up to 60% in certain groups, with a meaningful proportion of patients achieving remission. Outside depression, TMS is now applied to conditions such as migraines, chronic pain, PTSD, and even stroke rehabilitation, reflecting a growing body of evidence supporting its versatility.
Safety and Side Effects
TMS consistently demonstrates a high margin of safety in clinical research and real-world use. The most common side effects include mild scalp discomfort, slight headache, or muscle twitching during the actual stimulation. These side effects usually diminish over the course of treatment and rarely interfere with daily activities.
Critically, TMS is not associated with systemic side effects such as weight gain, sexual dysfunction, or sedation, which frequently impede antidepressant medication use. For patients needing safe, outpatient care, TMS represents a practical choice.
Advancements in TMS Technology
Continued research has spurred the evolution of new TMS technologies. The advent of Deep TMS—utilizing specialized H-coils—enables clinicians to target deeper brain structures, potentially those associated with more severe or complex psychiatric symptoms.
Deep TMS is FDA-approved for both depression and obsessive-compulsive disorder, and ongoing studies aim to refine stimulation protocols to maximize benefit for individuals with diverse diagnoses. Technological innovation also enhances treatment speed, comfort, and targeting, thereby expanding the accessibility and applicability of TMS.
Conclusion
Transcranial Magnetic Stimulation stands at the intersection of neuroscience, physics, and compassionate care. As a non-invasive, evidence-supported therapy, TMS gives hope to those with stubborn mental health challenges, providing a pathway to improved mood, function, and overall quality of life.
As emerging research continues to clarify and expand its uses, TMS is poised to play a key role in the evolving landscape of mental health treatment.